This is an approximate transcript of the presentation given by Mark E Thomas at the launch, hosted by Richard Burgon, MP on 4 July.
Present from Parliament were MPs Caroline Lucas (Leader Green Party), Margaret Greenwood (Labour MP for Wirral West) Mary Kelly Foy (Labour MP for Durham), Kenny MacAskill (Alba Party); Ian Byrne (Labour MP for Liverpool, West Derby), Micky Brady (Sinn Fein MP for Newry and Armagh), Rachael Maskell (Labour (Co-op) MP for York Central),Liz Saville Roberts (Plaid Cymru MP for Dwyfor Meirionnydd); and Members of the House of Lords Baroness Golding (Labour Peer), Baroness Walmsley (Lib Dem Peer), and Lord Dubs (Labour Peer).
Also present were members of The 99% Organisation, Keep Our NHS Public, Every Doctor, the National Health Action Party and We Own It.

Thank you very much Richard, and Good Afternoon, everyone.
As Richard said, I’m going to talk for about 20 minutes and then leave plenty of time for discussion, but before that, let me introduce the panel.
We have Professor Patricia Murray, who began her career as a nurse and is now Professor of Stem Cell Biology at the University of Liverpool. Patricia has personal experience of what works well in healthcare innovation as well as the potential for abuse.
Doctor Tony O’Sullivan was an NHS Consultant Paediatrician until 2016; and he has been Co-chair of Keep Our NHS Public since 2015. Tony’s practical experience of what works and what does not work in private sector involvement with the NHS is unmatched.
Chris Banks has been – among other things – Chief Executive of the Northwest Anglia NHS Foundation Trust, Chief Executive of NHS Cambridgeshire and Chief Executive of Tower Hamlets GP care group. He has 30 years’ experience of the practicalities of managing the NHS through good times and bad.
Before we give them a chance to answer your questions, let me quickly run through the key points of our report.
When the NHS was founded, it was a central part of the UK’s post war social contract. Now, it is struggling to perform and there are increasing calls for so-called ‘reform’ which is often a euphemism for further privatisation and introduction of some form of insurance-based funding. There are increasing calls, in other words, for a fundamental change to the business model of the NHS – a public service, free at the point of use and funded through progressive taxation.
Given the importance of this issue we decided to take a look at the facts – what is the rational way forward for the UK? We pulled together a team of volunteers with expertise ranging from NHS management and senior clinical roles through to strategy, economics and financial analysis. This team has produced a report, The Rational Policy Maker’s Guide to the NHS, timed to coincide with the anniversary.

I know you are all rational policy makers. Imagine specifically that you were a rational policy maker who had been given the challenge of charting the future course of healthcare in the United Kingdom.
How would you go about it?
You would probably ask yourself three questions:
- What works in practice? – When you look around the world at the different systems in place in different countries, which ones actually perform for their citizens?
- What has gone wrong in the UK? – There is no disputing the fact that the NHS is now struggling badly; what is the root cause of that struggle?
- What kind of system would be sustainable into the distant future? – Given that the UK has a growing and ageing population, what strategy is most likely to stand the test of time?
And those are exactly the questions the team addressed.
Let me take you quickly through what we found, and then we can discuss the issues in more detail.
What works in practice?
Of course, healthcare systems are enormously complex and there are many ways to assess their performance. From the point of view of citizens of a country, there are three main things we can ask of our healthcare system:
- first of all, we want it to be effective – when we are ill, we want it to deliver high-quality healthcare at least on a par with what citizens of other wealthy countries receive;
- Secondly, we want it to be equitable – the quality of care we receive should not depend on how wealthy we are or how important we are perceived to be; all citizens should have the same right to high quality healthcare;
- And finally, since we are taxpayers, we want it to be efficient. The definition of efficiency is output (quality of care provided) divided by input (principally money) – we should not be spending more than other countries for the same standard of healthcare.

That’s what we can ask, but it is not all we care about. If the inputs are not there, the outputs will be poor. And context matters: the US has very poor life expectancy compared with other countries, and part of that is certainly down to healthcare – but a big part is gun-crime, overdoses, and other ‘external’ causes.
So benchmarking healthcare systems is complex. Fortunately, there are several established international benchmarks that we can look at. Of these, the most comprehensive are those produced by the Commonwealth Fund.
Here is a summary of the Commonwealth Fund’s analysis published in 2014, using data from 2011-2013.

As you can see, the benchmarking shows a clear #1 – the pre-underfunded NHS. Best on outputs – quality of care – best on efficiency, and excellent on equity. Not best on healthy lives because of the context of high levels of poverty and inequality.
It also shows a clear #11 – The US system, which is by far the worst in the developed world.
But that is just a snapshot. When we look over a longer time, what do we see?

The long-term picture is similar. The UK has slipped slightly in recent years and is no longer #1 (though it was still #1 as recently as 2017) – but overall, the UK has the best track record.
Why is this?
Well, the UK system naturally scores very well on equity. A system which is free at the point of use and funded from progressive taxation is the best way of delivering equitable health care.
It also scores extremely well on efficiency – indeed it has often been the most efficient system. This is both because of its scale which, for example, gives it enormous buying power, and because of the dedication of its staff many of whom have for decades known that they might be able to earn more elsewhere, but stayed with the NHS because they believed in it. We are now, of course, well beyond the point where governments can exploit this loyalty without consequence.

So, in summary, looking around the world to see what works in practice gives a clear answer: the pre-underfunded NHS is the best model so far demonstrated in an advanced economy.
A rational policy maker would start with that fact.
But he or she would still want to check the other two questions. So let’s take a look at what went wrong.
What went wrong?
In essence, the answer is very simple: underfunding. Since 2010, we have been spending less than other advanced countries, spending a declining percentage of GDP on healthcare, and – most importantly – not keeping pace with the needs of the UK population.

I won’t go through all the lines on this chart, but you can see the picture very clearly.
(Note that we have used pre-COVID data because the UK had a poor COVID response which added to the load, there was a significant amount of suspect spend, which is still under investigation, in response and there is a significant post-COVID load still being borne by the NHS. It would be difficult to correct for these factors).
You can see a noticeable change in funding policy from 2010 onwards. Before then, as with other countries, the UK had been spending a gradually increasing percentage of GDP on healthcare; since 2010 it has been a gradually decreasing percentage, and spending in the UK is now below almost all other advanced economies.
The other line which is worth looking at is the top line, the US. In terms of efficiency (as well as several other measures) the US system is by far the worst in the developed world. A rational policy maker would certainly not consider modelling the future healthcare system in the UK on the US system.
Most importantly, our spending is no longer keeping pace with need. The government claims that it is spending more than ever before on the NHS, but that is only true if you ignore the impact of inflation, a growing population, an ageing population and a population with increasing rates of ill health.

Of course, £1 in 2010 went much further towards meeting the needs of the UK population than £1 does in 2023. A rational policy maker would not ignore these other factors.
If we focus on the bottom line, the red line, which does take these factors into account, we see that whereas we had been increasingly able to meet need until the Global Financial Crisis struck, the NHS has been decreasingly able to meet need since then. And the results reflect that.

These charts show that both in terms of outputs such as the ability of the NHS to meet its waiting list targets and emergency admissions targets and in terms of outcomes such as life expectancy and avoidable mortality, the NHS has been increasingly struggling to perform since the underfunding began.
So, our rational policy maker would by now have established both that the pre-underfunded NHS was the best model so far demonstrated in an advanced economy and that the main reason for its underperformance in recent years is underfunding. On that basis alone, he or she might be tempted to conclude that the best strategy was to recommit to the fundamental business model over the NHS and to fund it properly.
But there is still the question of sustainability: the fact that the NHS was the best model for much of the previous 75 years does not guarantee that it will be sustainable for generations to come. So let us explore that point.
What about long term sustainability?
It is tempting to duck this question: we have already established that the NHS is the most cost-effective system in the countries studied – so if we can’t afford the most cost-effective system of universal healthcare, we are really saying that we can’t afford any system.
But we should not duck it: if there are problems of affordability in the future, we should start planning for them now. Fortunately, our analysis suggests no such problems.
To look at sustainability, we need to explore the linkages between the healthcare system and the wider economy over time, and when we start to do this, we see three important chains of cause and effect:
- Chain 1: the Capacity Loop:
- The economy is driven by people – specifically healthy people of working age;
- The number of healthy people of working age is driven by the treatment provided by the healthcare system as well as factors affecting rates of ill-health – around 2.5 million working age adults are currently unable to work due to ill-health, that’s 7% of the total, and rising fast;
- Capacity to treat (staff, hospital beds, technology, etc) is driven by funding;
- Funding is enabled by having a healthy economy.

So, on its own, that looks simple enough. But we need to consider other loops which interact with that one.
- Chain 2: the Poverty Loop:
- Poverty drives rates of ill-health;
- Rates of ill-health drives demand for treatment;
- Excess demand causes untreated illness;
- Untreated illness reduces number of healthy people;
- Reduced number of healthy people of working age decreases economic output;
- Economic output enables economic decisions to address poverty;

- Chain 3: the Prevention Loop
- Spending on prevention reduces illness;
- Reduced illness reduces need to treat;
- Reduced need to treat reduces funding requirement for treatment capacity;
- Reduced funding requirements makes adequate spending easier.
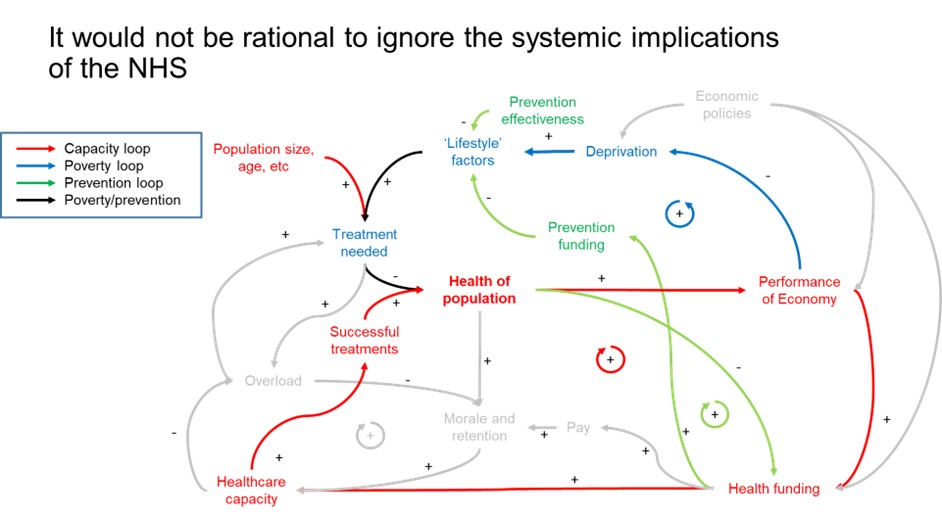
Unfortunately, most people – including policy makers – find the complete picture a bit frightening! And it’s very tempting to say, “that looks ridiculously complicated, I’m just going to use my common sense.”
But that doesn’t work: ignoring these loops doesn’t remove them from the real world. Many of you will have heard Sir Michael Marmot talking about his research into the social determinants of ill health. That is the poverty loop. If policymakers ignore that loop, the consequences don’t disappear, they get worse.
Fortunately, the discipline of system dynamics has developed over the last 70 years precisely to enable rational policy makers in business to tackle this kind of complexity.
We built a system dynamics model based on the 3 loops and used it to assess three types of policy:
- Different approaches to funding the NHS;
- Different approaches to poverty reduction;
- Different approaches to investment in prevention.
Let’s start with funding. We saw that since 2010 government policy on funding has been to gradually reduce spending on the NHS as a percentage of GDP. We do not know what the government’s end goal is, but we can model different levels of funding and trace their impact around the capacity loop.

And this is what we see: without significantly greater funding than today, the UK is highly unlikely to reach what the OECD forecast to be its GDP in the year 2060. Even worse, if the government were to pursue its policy of cost reduction into the future, we could be heading for a generation of zero growth – something unheard of in a modern developed economy.
In either case, current policies are pointing towards economic failure.
What is the alternative? Of course, there are many alternatives. We have modelled a scenario in which government policy has three strands:
- Fund the NHS in line with need;
- Increase spending on preventive health care;
- Use GDP growth to fund poverty reduction initiatives.

The results are extremely encouraging: although there is a need for significant increases in funding over the next few years – largely because of the need to rebuild capacity after the years of underfunding – in the long run, NHS funding will not need to increase as a % of GDP year on year. It is long-term sustainable.
This scenario also sees far better economic performance: with this policy, the UK will meet the OECD targets for GDP in the 2060.
In short, while a properly funded NHS is sustainable and is good for the UK economy; an underfunded NHS will mean a failing economy.
Conclusion
What our research has shown is, in essence, very simple: the pre-underfunded NHS was the best proven model for healthcare delivery; it has struggled because of prolonged and severe underfunding; and with proper funding it can be restored to its natural position as the world’s best healthcare system.
So the choice for rational policy-makers is stark: if we do not act, both the NHS and the UK economy will fail; if we do act, they can both thrive.
A recent IPSOS poll showed that 54% of Britons are prouder of the NHS than any other aspect of being British. History remembers fondly those rational policy-makers Keynes, Beveridge, Attlee and Bevan who enabled the foundation of the NHS. Let us make sure that we are remembered, not as the generation which blew it, but as the generation which saved the NHS and with it, the UK economy.
Thank you. I’m sure you’ve all got lots of questions!
You can read the full report here.
And, if you would like to help, you can join the 99% Organisation here.
3 comments so far
hi Mark, hadn’t seen the efficiency ratings before, nor a chart highlighting changes that included population growth. As always, absolutely outstanding work. Sorry I don’t see you in my timeline as much nowadays! I read your fantastic thread yesterday, of which this presentation is part of. Thanks as always!
It is very encouraging to see that policy makers really do want more rational and systemic approaches to this horribly complex challenge. This is a helpful first step.
Another piece of brilliant work. Bravo Mark and team! Reassuring that informed people are thinking long term. Hope the message is heard. Standing room only in the committee room; says a lot! Very proud to be involved, even in a tiny way, with this very important movement: 99%. CM